Guided bone and tissue regeneration is a surgical method that enhances healing in bone and tissue defects‚ commonly used in dental implants and periodontal treatments to restore lost structures․
1․1 Definition and Overview
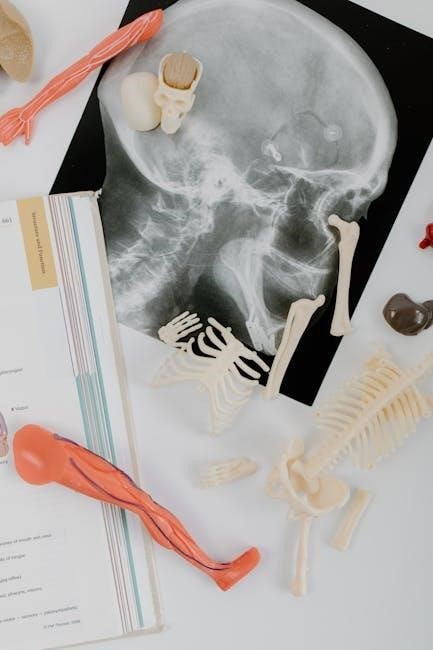
Guided bone and tissue regeneration (GBR) is a surgical procedure that enhances bone healing in deficient areas‚ typically for dental implants․ It involves using barriers and biomaterials to direct the body’s natural repair processes‚ ensuring proper bone regrowth․ This technique is vital for restoring functional and aesthetic outcomes in patients with bone loss‚ guiding the body to regenerate tissue effectively without interference from soft tissue ingrowth․
1․2 Historical Development
Guided bone and tissue regeneration emerged in the mid-20th century‚ with early concepts focusing on bone grafting and barrier membranes․ Significant advancements occurred in the 1980s‚ introducing resorbable materials and growth factors․ The 1990s saw the integration of biomaterials and tissue engineering‚ enhancing predictability․ Modern techniques incorporate 3D printing and stem cell therapies‚ pushing the boundaries of regenerative medicine and improving patient outcomes in dental and orthopedic applications․
1․3 Importance in Dental and Orthopedic Applications
Guided bone and tissue regeneration is crucial in dental applications for implant placement and treating periodontal defects․ It restores lost bone and tissue‚ ensuring implant stability․ In orthopedics‚ it aids in repairing fractures and bone defects‚ promoting natural healing․ This technique enhances both functional and aesthetic outcomes‚ making it a cornerstone in modern reconstructive surgeries across dental and orthopedic fields․

Fundamental Principles of Guided Bone and Tissue Regeneration
Guided bone and tissue regeneration relies on biological healing processes‚ utilizing biomaterials and growth factors to promote cell differentiation and tissue formation‚ enhancing natural repair mechanisms effectively․

2․1 Biological Basis of Bone and Tissue Healing
Bone and tissue healing is a complex biological process involving cell proliferation‚ differentiation‚ and extracellular matrix formation․ Osteoblasts and stem cells play pivotal roles in bone regeneration‚ while collagen and growth factors facilitate tissue repair․ The body’s natural repair mechanisms are enhanced through guided regeneration techniques‚ ensuring a stable environment for new tissue and bone growth‚ critical for successful dental and orthopedic outcomes․
2․2 Role of Biomaterials in Regeneration
Biomaterials are essential in guided regeneration‚ providing a scaffold for cell attachment and tissue growth․ They include autografts‚ allografts‚ xenografts‚ and synthetic materials like hydroxyapatite and titanium․ These materials promote osteoconduction‚ osteoinduction‚ and osteogenesis‚ enhancing bone healing․ Their porosity and biocompatibility facilitate cell migration and vascularization‚ while resorption rates ensure temporary support without hindering permanent tissue formation‚ making them critical for successful bone and tissue regeneration outcomes․
2․3 Significance of Growth Factors and Signaling Pathways
Growth factors‚ such as BMPs and PDGF‚ play a pivotal role in regeneration by signaling cells to differentiate‚ proliferate‚ and migrate․ They regulate osteogenesis and angiogenesis‚ essential for tissue repair․ Signaling pathways like Wnt and TGF-β activate cellular responses‚ promoting bone and tissue formation․ These biological cues enhance healing efficiency‚ ensuring proper integration of biomaterials and grafts‚ making them indispensable in guided regeneration therapies for dental and orthopedic applications․

Applications of Guided Bone and Tissue Regeneration
Guided bone and tissue regeneration is widely applied in dental implantology‚ periodontal disease treatment‚ and orthopedic surgeries‚ repairing bone defects and promoting tissue repair effectively․
3․1 Dental Implantology and Periodontal Disease Treatment
Guided bone and tissue regeneration is crucial in dental implantology‚ enabling successful implant placement in deficient jawbones․ It also treats periodontal disease by repairing bone loss around teeth‚ stabilizing them‚ and preparing the jaw for implants‚ ensuring long-term oral health and function․
3․2 Orthopedic and Maxillofacial Surgery
Guided bone and tissue regeneration is vital in orthopedic and maxillofacial surgery for repairing bone defects caused by trauma‚ tumors‚ or congenital anomalies․ Techniques like bone grafting and biomaterials help restore structural integrity‚ enabling proper healing and functional recovery․ In maxillofacial surgery‚ it addresses defects in the facial bones‚ improving aesthetics and function‚ often in cases of severe injuries or reconstructive procedures․
Biomaterials Used in Guided Bone and Tissue Regeneration
Biomaterials are crucial in guided regeneration‚ including autogenous grafts‚ allografts‚ xenografts‚ and synthetic options‚ each offering unique benefits for bone and tissue repair․
4․1 Autogenous Bone Grafts
Autogenous bone grafts‚ harvested from the patient’s own body‚ are the gold standard for bone regeneration due to their high osteoconductive and osteogenic properties‚ ensuring optimal healing and integration․
4․2 Allografts and Xenografts
Allografts‚ derived from donor bone‚ and xenografts‚ sourced from non-human species‚ are widely used in bone regeneration․ They eliminate the need for a second surgical site‚ reducing patient morbidity․ These grafts serve as osteoconductive scaffolds‚ promoting bone healing and integration․ Allografts are treated to remove organic components‚ while xenografts retain their mineral structure․ Both are effective in repairing bone defects and preparing the jaw for dental implants‚ offering a biocompatible and safe alternative to autografts․
4․3 Synthetic and Bioactive Materials
Synthetic and bioactive materials‚ such as hydroxyapatite‚ calcium phosphates‚ and bioactive glasses‚ are engineered to mimic natural bone structure; These materials are osteoconductive‚ supporting bone cell growth and tissue integration․ They are biocompatible‚ reducing immune responses‚ and can be designed to release growth factors‚ enhancing regeneration․ Synthetic grafts offer consistent quality and availability‚ making them ideal for dental and orthopedic applications where traditional grafts may be limited or impractical․
4․4 Advances in Scaffold Design and Tissue Engineering
Advances in scaffold design and tissue engineering have revolutionized guided bone and tissue regeneration․ Techniques like 3D printing enable precise‚ customized structures‚ promoting cell proliferation․ Biocompatible‚ bioactive materials and growth factors enhance tissue integration․ These innovations improve bone and tissue repair‚ offering solutions for complex defects․ Integration of stem cell therapies further boosts regeneration efficiency‚ making these scaffolds indispensable in modern surgical practices․
Growth Factors and Their Role in Regeneration
Growth factors‚ such as BMPs and PDGF‚ play a crucial role in bone and tissue regeneration by stimulating cellular proliferation and differentiation‚ enhancing healing processes․

5․1 Bone Morphogenetic Proteins (BMPs)
Bone Morphogenetic Proteins (BMPs) are a group of growth factors in the TGF-beta superfamily that play a key role in bone formation and healing․ They were first identified for their ability to induce bone growth by recruiting and differentiating mesenchymal cells into osteoblasts․ BMPs are widely used in bone grafting procedures to enhance bone regeneration by promoting a biological environment conducive to new bone tissue formation‚ making them essential in orthopedic and dental surgeries․
5․2 Platelet-Derived Growth Factor (PDGF)
Platelet-Derived Growth Factor (PDGF) is a potent growth factor that plays a critical role in tissue repair and regeneration․ It is derived from platelets and stimulates the proliferation and differentiation of cells‚ including fibroblasts‚ osteoblasts‚ and mesenchymal stem cells; PDGF enhances bone and tissue regeneration by promoting angiogenesis and collagen synthesis‚ making it a valuable component in periodontal and orthopedic therapies‚ often used in combination with other growth factors for synergistic effects․
Surgical Techniques and Procedures
Surgical techniques in guided bone and tissue regeneration involve the use of barrier membranes‚ bone grafts‚ and growth factors to promote healing and new tissue formation․

6․1 Guided Bone Regeneration (GBR) Techniques
Guided Bone Regeneration (GBR) involves using barrier membranes to direct bone growth‚ often combined with bone grafts and growth factors․ This method is commonly employed in dental implant placements and periodontal defect treatments․ The membrane prevents soft tissue invasion‚ allowing bone to regenerate in deficient areas․ Surgical steps include membrane placement‚ graft stabilization‚ and ensuring a healing-friendly environment․ GBR typically requires 3-6 months for bone maturation before implant placement‚ with growth factors sometimes used to enhance bone formation․
6․2 Guided Tissue Regeneration (GTR) Methods
Guided Tissue Regeneration (GTR) employs barrier membranes to promote healing in periodontal pockets‚ preventing epithelial invasion․ This method allows the body to regenerate lost tissue naturally․ GTR is widely used in treating periodontal defects‚ enhancing tissue repair‚ and improving dental implant success rates by creating a favorable environment for tissue growth and attachment․
6․3 Minimally Invasive Approaches
Minimally invasive techniques in guided bone and tissue regeneration focus on reducing surgical trauma and recovery time․ These methods utilize advanced tools and materials‚ such as resorbable membranes or growth factors‚ to promote healing with minimal tissue disruption․ Approaches like laparoscopic surgery or small-incision procedures are employed to enhance patient comfort and improve outcomes‚ ensuring faster recovery while maintaining effective tissue and bone regeneration․

Complications and Risks
Complications may include implant rejection‚ adverse reactions to biomaterials‚ or incomplete regeneration due to surgical errors or insufficient bone density‚ requiring careful monitoring and treatment․
7․1 Common Surgical Complications
Common surgical complications in guided bone and tissue regeneration include infection‚ graft rejection‚ and incomplete healing․ Infection can arise from improper sterilization or patient-related factors․ Rejection of biomaterials or grafts may occur due to immune responses or poor material compatibility․ Additionally‚ surgical errors‚ such as improper placement‚ can lead to failed regeneration․ Patient-specific factors‚ like smoking or diabetes‚ may also hinder healing‚ necessitating careful preoperative planning and postoperative care to minimize risks․

7․2 Management of Infections and Graft Failures
Infections and graft failures in guided bone and tissue regeneration require prompt intervention․ Antibiotic therapy is often the first line of treatment‚ while surgical debridement may be necessary to remove infected or necrotic tissue․ Failed grafts can be addressed by re-evaluating biomaterial compatibility and ensuring proper surgical technique․ Preventive measures‚ such as strict sterilization protocols and patient monitoring‚ are crucial to minimize these complications and improve long-term outcomes․

Current Research and Advancements
Recent advancements in guided bone and tissue regeneration include stem cell therapy‚ 3D printing‚ and bioprinting‚ offering innovative solutions to enhance precision and patient outcomes․
8․1 Stem Cell Therapy in Regeneration
Stem cell therapy is revolutionizing guided bone and tissue regeneration by utilizing mesenchymal stem cells to differentiate into bone and tissue cells‚ enhancing healing and reducing recovery times․ Researchers are exploring its potential in dental and orthopedic applications‚ leveraging its ability to promote natural tissue repair․ This approach offers personalized treatment options‚ improving outcomes for patients with bone defects or degenerative conditions․ Advances in stem cell therapy are paving the way for more effective and minimally invasive regenerative solutions․
8․2 3D Printing and Bioprinting in Tissue Engineering
3D printing and bioprinting are advancing tissue engineering by creating customized scaffolds for bone regeneration․ These technologies enable precise implant designs tailored to patient needs‚ incorporating growth factors to enhance healing․ They are particularly effective in treating large bone defects‚ reducing the necessity for multiple surgeries and improving patient outcomes significantly․
Guided bone and tissue regeneration is a transformative approach in dental and orthopedic treatments‚ offering innovative solutions for tissue repair․ Future advancements in biomaterials and growth factors will further enhance its potential‚ paving the way for more efficient and personalized therapies․
9․1 Summary of Key Concepts
Guided bone and tissue regeneration combines biological processes‚ biomaterials‚ and surgical techniques to repair defects․ It leverages growth factors and scaffolds to enhance healing․ Key applications include dental implants and orthopedic repairs․ The use of autografts‚ allografts‚ and synthetic materials has revolutionized treatment outcomes․ Advances in stem cell therapy and 3D printing promise further innovation․ Understanding these concepts is essential for advancing regenerative medicine and improving patient care in both dental and orthopedic fields․
9․2 Emerging Trends and Innovations
Emerging trends include advancements in 3D printing and bioprinting for customized scaffold designs․ Stem cell therapies and bioactive materials are being explored to enhance regeneration․ Personalized medicine approaches are also on the rise‚ offering tailored treatments․ These innovations aim to improve efficiency‚ reduce recovery times‚ and provide more effective outcomes for patients․ The integration of cutting-edge technologies promises to revolutionize the field‚ making regenerative procedures more accessible and successful․
